Background Information
Percutaneous Coronary Intervention (PCI) is a non-surgical procedure to treat many types of heart issues using thin flexible tubes (catheters), guidewires (wires that are used as a guide for placement of other medical devices), and stents (small structures to prop open the blood vessel).
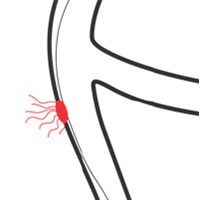 One unlikely complication of a PCI procedure is a perforation (hole) in the vessel. A perforation can occur when a catheter, guidewire, or other medical device, such as a stent, gets caught in the vessel wall and pushes through the wall to create a hole that allows blood to escape the vessel. This is a rare, life-threatening complication that may result in significant blood loss and potentially death.
One unlikely complication of a PCI procedure is a perforation (hole) in the vessel. A perforation can occur when a catheter, guidewire, or other medical device, such as a stent, gets caught in the vessel wall and pushes through the wall to create a hole that allows blood to escape the vessel. This is a rare, life-threatening complication that may result in significant blood loss and potentially death.
Current Treatment
There currently are no commercially available devices that temporarily control bleeding through the perforation (hole) in the vessel during coronary perforations.
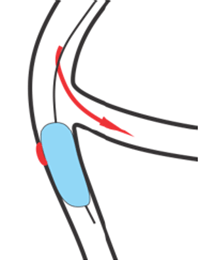 Bleeding through the perforation (hole) in the vessel can be controlled with a standard balloon catheter, but when standard balloons are inflated, the balloon also blocks blood flow through the vessel. This blockage of blood flow can lead to a heart attack (death of part of the heart’s muscle). Because standard balloons block blood flow, they should only be inflated for short periods of time. If the balloon needs to be deflated before the perforation can be treated, blood loss may continue to occur through the perforation.
Bleeding through the perforation (hole) in the vessel can be controlled with a standard balloon catheter, but when standard balloons are inflated, the balloon also blocks blood flow through the vessel. This blockage of blood flow can lead to a heart attack (death of part of the heart’s muscle). Because standard balloons block blood flow, they should only be inflated for short periods of time. If the balloon needs to be deflated before the perforation can be treated, blood loss may continue to occur through the perforation.
To permanently seal the perforation (hole) in the vessel, a covered stent (flexible tube that is permanently placed in the vessel) may be placed, or the patient may be sent to surgery for an emergency coronary artery bypass graft (CABG) surgery. A CABG surgery involves using veins from your leg or arm or arteries from inside your chest to bypass the hole.
Investigational Device
The Ringer™ Perfusion Balloon Catheter
is intended to control bleeding  until the
permanent treatment is determined.
Depending on the treatment required, the
Ringer™ Perfusion Balloon Catheter can be
inflated for one hour while the permanent
treatment is determined.
The Ringer™ Perfusion Balloon Catheter
controls bleeding from a perforation (hole)
in the same way as a standard balloon
catheter but has a balloon with a hollow
center that is designed to control blood
exiting the perforation while allowing
blood to flow through the vessel. This
means that the Ringer™ Perfusion Balloon
Catheter's balloon can be inflated for an extended period of time, controlling
bleeding from the perforation without blocking blood flow through the vessel.
until the
permanent treatment is determined.
Depending on the treatment required, the
Ringer™ Perfusion Balloon Catheter can be
inflated for one hour while the permanent
treatment is determined.
The Ringer™ Perfusion Balloon Catheter
controls bleeding from a perforation (hole)
in the same way as a standard balloon
catheter but has a balloon with a hollow
center that is designed to control blood
exiting the perforation while allowing
blood to flow through the vessel. This
means that the Ringer™ Perfusion Balloon
Catheter's balloon can be inflated for an extended period of time, controlling
bleeding from the perforation without blocking blood flow through the vessel.
Clinical Investigation
The Ringer™ Perfusion Balloon Catheter Clinical Investigation is a prospective, multicenter, single-arm clinical investigation intended to evaluate the safety and efficacy of the Ringer™ Perfusion Balloon Catheter. The only experimental part of the clinical investigation is use of the Ringer™ Perfusion Balloon Catheter Clinical Investigation for the control of bleeding from a perforation (hole). Patients in the clinical investigation will be undergoing a standard, non-experimental PCI procedure to treat an existing heart issue. In the unlikely event of a perforation, the physician will determine if the Ringer™ Perfusion Balloon Catheter can be used to appropriately control bleeding from the perforation. If the physician believes that it can be, the Ringer™ Perfusion Balloon Catheter will be delivered to the site of the perforation and inflated until a definitive treatment (such as placement of a covered stent) is determined.
Patients enrolled in this clinical investigation will be those who have a hole (coronary perforation) in their vessel during a PCI procedure where the physician determines that use of the Ringer™ Perfusion Balloon Catheter is appropriate. Patients will only be enrolled through hospital discharge or 24-hours post-procedure (whichever comes first). If a patient is enrolled, FDA may inspect their records related to the clinical investigation.
The clinical investigation is expected to enroll 30 patients and last approximately 17 months after IRB approval to begin enrollment.
Exception from Informed Consent
The clinical investigation will be conducted in accordance with special regulations for emergency research. Under these regulations, patients can be enrolled in the clinical investigation without their consent if certain criteria are met.
These emergency research regulations apply in cases where patients are in a life-threatening emergency and it is not possible to obtain informed consent. The regulations also require that there is no reasonable way to identify patients likely to become eligible for the clinical investigation and that the clinical investigation could not practicably be carried out without the exception.
The regulations will apply to this clinical investigation because a perforation (hole) can be a life-threatening emergency that needs to be immediately controlled, and there is not enough time for the patient (who is likely under sedation) or his/her legally authorized representative or family member (who is not in the operating room) to give consent. Perforations occur in less than 1% of cases and are not specific to any type of PCI procedure, meaning there is no reasonable way to identify patients ahead of time. It is estimated that over 14,000 PCI patients would need to be approached for the clinical investigation in order to enroll the 30 patients intended to be enrolled in the clinical investigation. This burden on the clinical investigation staff and hospitals makes the clinical investigation not practicable without the waiver.
Patients may choose to withdraw from the clinical investigation at any time without penalty.
Risks and Benefits
There are no guaranteed benefits from use of the Ringer™ Perfusion Balloon Catheter. However, it is possible that use of the Ringer™ Perfusion Balloon Catheter may provide a lower-risk catheter-based means of controlling the loss of blood from a perforation (hole) compared to currently available devices and treatments. Additionally, because RINGER’s balloon is hollow, physicians can also deliver other interventional devices through it and potentially advance progress of a PCI procedure. This may eliminate the need to perform a follow-up procedure.
There are risks associated with all procedures that use medical devices to treat a diseased heart and associated blood vessels. It is believed that the risks associated with use of the Ringer™ Perfusion Balloon Catheter are similar in nature and frequency to the risks of the PCI procedure in general. The frequency and severity of adverse events can vary, and may require additional medical intervention, including surgery.
Clinical Investigation Costs
In this clinical investigation, the only ‘investigational’ part of the procedure is the use of the Ringer™ Perfusion Balloon Catheter. In the event there is a complication during a regularly scheduled PCI procedure, the complication results in the use of the Ringer™ Perfusion Balloon Catheter, and the patient’s insurance will not cover the use of the investigational device during management of the complication, the clinical investigation sponsor will cover the cost of the use of the Ringer™ Perfusion Balloon Catheter device and any device related complications. The clinical investigation sponsor will also cover the costs associated with the certain lab tests as, even though they are standard of care for a PCI procedure, the protocol dictates the specific timing of the tests.
The patient’s insurance company will still be responsible for the costs of the PCI procedure and all standard-of-care tests, visits, and medications as they normally would for a PCI procedure. These costs will include their usual insurance deductibles and co-payments. All of the patient’s insurance company’s usual rules would apply.
In some cases, insurers may not reimburse claims submitted for standard-of-care medical items, procedures, or treatments if they are performed as part of a research clinical investigation. Prospective patients may want to talk with their insurance company about its payment policy for standard medical care given during a research clinical investigation. If the insurance company does not pay, the patient may be billed for those charges.
Opportunity for Input
Because this clinical investigation will be conducted under special regulations for emergency research, it is important for any concerns from the community in which the clinical investigation is being conducted to be heard and incorporated into the clinical investigation. You are encouraged to provide feedback on this planned clinical investigation by contacting Vascular Solutions/Teleflex or the participating site using the contact information provided in this brochure.